How to support effective recovery for children who have experienced trauma
Aug 18, 2021
Trauma doesn't care about your colour, race, gender, ethnicity, size or age. We will all experience trauma at some stage in our lives. However, the earlier it occurs, the more damaging it can be.
Why?
Because like a seed, when planted in the fertile soil of a young child's mind, the trauma will shape how that child's brain develops. What neural networks or connections in the brain are formed. What memories are retained and what meanings are assigned to those memories.
Previously we went into detail about the four basic elements necessary for a trauma to be encoded in your mind and then discussed the outflows - or how we respond to trauma.
What happens when a child experiences a trauma
When we are children, we have very limited cognitive resources, such as emotional awareness and thought management, as well as limited experience to help us in our decision making with regards to perceived threats.
When a child experiences a trauma (which is linked to the loss of something or someone), their chosen response can be one of three pathways:
- Automatic - based on their genetic makeup, as encoded in their genes from past generational responses to trauma, triggered by their environment
- A learned choice - based on how they have observed others respond to a similar experience within their social environment
- A personal choice - based on what they think is appropriate at the time, with no previous learning.
What is markedly different between a child's and an adult's response is their level of cognitive maturity.
For example, a child that experiences a trauma pre-birth or during birth will not have the language skills or basic emotional regulation to articulate or understand what is happening.
Their brain simply does not have the neural networks (connections) present to join the dots between the decided response and what that means cognitively - they can't assign thought, words and images to their chosen response.
Pre-language, children tend to respond to trauma or unhelpful experiences physically. If a child is behaving aggressively, get curious about the source - it is most likely unregulated past or present trauma.
In terms of the four outflows when we experience a trauma, early childhood responses are mainly autonomic and somatosensory in nature, with the emotional content expressed physically rather than verbally.
From an autonomic perspective, the child may experience an increase in heart rate, blood pressure, breathing, body temperature may reduce, they may show pupil dilation and all of this will result in increased cortisol levels.
From a somatosensory perspective, the child may experience unexplained pain, tingling, numbness, desire to grind teeth, feeling off balance, tics or stuttering, shaking, wanting to freeze or lash out.
Our emotions are essentially a signal for our body to 'do something' to release the energy associated with that emotion.
From an emotional perspective, trauma-encoded responses in children are typically physical in nature. Rage, anger, fear, frustration may all result in the child 'lashing-out' to expel the negative energy associated with that emotion. Upsetting scenes or fear may result in uncontrollable crying.
This is why traditionally 'talk' therapy can be ineffective for anyone who has experienced childhood trauma. Before the age of seven children are still building the neural networks in their brain to connect their experienced emotions with the language associated with those emotions through a region of the brain called the corpus callosum.
Our brains don't fully mature until the age of 25 years old on average for females and 28 years old on average for males.
During theses developmental years our brains are emotionally charged as the older regions of our brains come online first, with the newer regions of our brain - the Prefrontal Cortex, or executive function responsible for planning, logic and decision making coming online last.
This is why appropriate parental or carer support is vital during our teenage years.
The deep limbic system that houses our amygdala (often cited the reptilian part of our brain - the oldest part of our brain), which is essential to our survival as a species and where we initiate our response to trauma via fight/flight/freeze/defensive rag, comes online first. Neurons that comprise the structures of this system are generated within the first two weeks of gestation.
When the child feels in a 'safe' environment to express their emotions, or the expression is a means to escape the trauma or release the encoded response from a trauma following a triggering event, you may witness any of the above releases.
When the child feels 'unsafe' to express their emotions, you may witness a child becoming more withdrawn, quiet and reserved.
A child will do whatever they feel is appropriate to aid their survival.
In times of conflict, war, natural disasters, or other events that involve both adults and children witnessing, hearing or experiencing a trauma collectively, how the adult responds will directly influence a child's response.
From birth children are dependent on a carer for their emotional regulation until they have the ability to self-regulate their emotions.
If an adult carer is 'scared,' the child may no longer feel 'safe' emotionally, physically, mentally or spiritually to express themselves and release the outflow they need to let go of the trauma - to escape.
Often when this happens, the child seeks to create a 'safe Haven' for themselves or for the carer to help that carer down regulate. This is ultimately essential for the child's survival - for if the carer can't care and provide that emotional regulation, the child can't survive.
So what are the key steps we can take to support the effective recovery for children who have experienced trauma?
Step 1 - Unchain your pain and break the bonds from past generational trauma
Understand the importance carers - parents, nurseries, schools, professionals, community support groups and organisations that interact with children, play in supporting a child's emotional development and regulation.
To provide that safe, nurturing, emotionally supportive environment, it's vital we address our own emotional irregularities and heal from any past traumas and unchain our pain first. As they say 'put your oxygen mask on first before attempting to help others.'
This is about addressing the first of the three pathways by unchaining the pain from past generational trauma. Genes only load the gun, our environment pulls the trigger.
Step 2 - Create an emotionally safe environment to learn and grow
Create an emotionally safe environment for that child to feel able to express themselves and learn how to manage their emotions.
Destabilising emotional environments can be created when:
- Carers mistake quantity of time over quality time with their child - limiting emotional bonding
- Carers are unable to manage their emotions when the child can't manage theirs, e.g. being kind one second and exploding in rage another. This causes the child confusion and doesn't create a safe emotional space for that child
- Exposing children to distressing news (radio/TV) or social media channels that create fear and emotional unease, without offering emotional support or regulation
- Carers spending time 'talking' about their fears in the presence of the child, forgetting that the child is always listening, always learning, but not always able to verbally express what they've learnt.
On average it takes 11 years between a child expressing symptoms of mental health before they receive appropriate treatment. 75% of mental illnesses are thought to start before the age of 25 years old.
Often mental health struggles can be attributed to some form of childhood trauma. This trauma can often be missed because:
- Carers believe that the child has to 'tell you' there's something wrong for there to be something wrong
- The child is unable to explain how they feel
- The child feels ashamed of what has happened
- The carer is not a 'safe emotional person' for the child to talk to
- The child has communicated their fears in different outflows to 'talking' but the carer has simply not recognised them.
When I was a child at about 10 years old I spoke to my mum about a trauma I had experienced. She has no recollection of that conversation. I remember the discussion to this day. It was a really difficult one to have. I didn't feel heard at the time and so went inside my mind to protect myself. Ultimately I don't think she understood what I was trying to say.
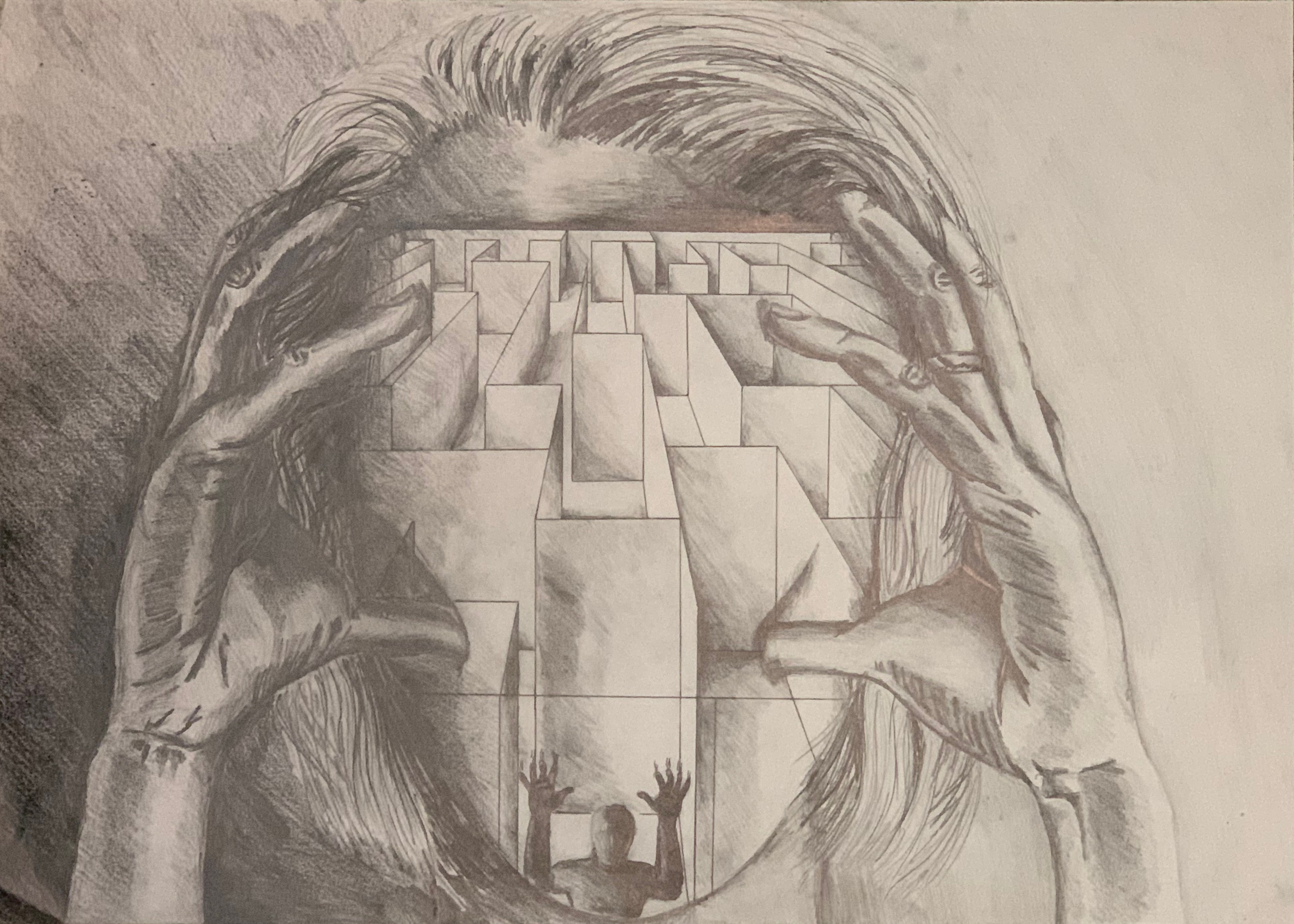
Later on in life I expressed how I felt in art. It was the final image for my Art GCSE. Unfortunately my mum just thought it was a piece of art, and only recently was I able to tell her that the picture was me, trapped inside my mind.
Be aware of signs beyond the verbal cues. These can include:
- Changes in behaviour - such as becoming withdrawn, not wanting to talk about emotions or having limited expression of emotions, emotional or aggressive outbursts without explanation, or excessive use of social media as an outflow
- Written word or dark images in journals or books, including doodling and artwork.
It's vital during the early childhood years that as a parent you create that 'safe haven' for your child to be able to express their emotions. This starts by spending quality time together where you give them your full attention.
Step 3 - Educate children on appropriate techniques to best manage their emotions
We can't be an emotional blanket for our children forever. So it's vital we equip our children with effective tools and techniques to better manage their emotions that they can use for life.
The below techniques are all underpinned by science as proven ways of calming the mind.
One of the simplest techniques is breath work. Regulating our breath helps regulate our autonomic nervous system.
Bring the child's attention to their breath. Get them to notice how their breath changes with exercise or activity. Show them how to regulate their breath - breath in for two seconds, breathe out for four seconds. Repeat up to 10 times or until they feel calmer.
I have a Yoga book at home and my daughter Lilly, aged 2, practises her breath work at the start and end of each Yoga session. She chooses the moves she wants to do - she loves 'Mighty Warrior' and 'Hissing Cobra'!
Meditation is another great way to help children regulate their emotions. This can simply be lying down next to your child and getting them to notice every part of their body, from head to toe and listening to their thoughts. Not challenging them, just being aware of them and letting their thoughts rumble on by.
Finally, Havening Techniques® is a fantastic approach to help children manage their emotions. This technique is excellent in helping children and adults let go of past trauma or unhelpful experiences, as you don't have to say anything about your experience to feel the benefit.
Not only can the relief be experienced in less than 30 minutes, but it is something that you can do together to nursery rhymes. My daughter Lilly learnt this aged 18 months and loves receiving Havening Touch before bed to calm her mind.
If you'd like support for you or those you care about, learn more and connect with us here.
You can teach your child how to self-Haven to nursery rhymes with our daughter Lilly here.
Further support
If you or children in your care are struggling with a past trauma or unhelpful experience and would like further support, please contact us now to arrange a free 15 minute consultation to discuss your needs.
Programs focused on supporting children in taking charge of their wellbeing are available through The Wellbeing Warrior Academy.
You are not stuck with the brain you have, you can make it better. Let us support you and show you how.


